
LITERATURE REVIEW
Psychosocial Impact on Medical Personnel Fighting
the Corona Pandemic – a Systematic Literature Review
Gerd D. Willmund a, Yasmin Youssef a, Christian Helms a, Antje Buehler a,
Peter Zimmermann a, Ulrich Wesemann a
a Bundeswehr Hospital Berlin, Psychotrauma Centre
Summary
Background: The current SARS-CoV2 pandemic poses a challenge for global health systems and the medical staff.
Objective: We wanted to find out if there are specific psychological symptoms that can be related to the current pandemic by conducting a systematic analysis of current literature.
Methods: In accordance with the PRIMSA guidelines, the PubMed database was systematically searched for clinical cross-sectional and prospective longitudinal studies that examined the psychosocial stressors of medical staff employed in the current pandemic. 29 of the screened 414 studies were included in our analysis after removing duplicates and studies without original data.
Results: Across all included studies, the medical staff showed psychological symptoms e.g. anxiety and depressive disorders, insomnia and stress or stress-reactive disorders with gender and profession related differences in prevalence.
Conclusion: A COVID-specific psychosocial burden on the medical staff is to be assumed, which is greater, especially when the regional pandemic situation is less uncontrollable.
Introduction
Since December 2019 the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV2) and the thereby caused respiratory distress syndrome COVID -19 pose a challenge for international health care systems. Globally 12 million infections have been confirmed. More than 500.000 deaths directly linked to the virus pandemic have been reported, with an even higher projected number of unreported cases. Economic and political consequences of the pandemic are currently subject of discussion in both media and politics and the pathway for infections as well as symptoms and possible treatment options are being discussed intensively. Opposingly the services and daily challenges faced by people working in the healthcare sector are not in the focus of interest and are only touched briefly in media coverage. Patient care had to be continued despite of the “lockdown”, while other professional groups were able to work in home-office. Private family challenges including the organization of childcare and “home schooling” and the care of old, diseased or disabled family members posed an additional burden that had to be managed parallel to occupation, especially for single parents. The onset of a new virus infection with unclear etiology and long-term health effects can cause feelings of distress and fear towards the disease, especially for people working in the medical and healthcare sector as they are potentially constantly in contact with infected patients. Usually, the risk of infection during daily activities or during work is controllable, if personal protective equipment is provided and used consequently and hygiene measures are adhered to. Feelings of distress can be intensified by lacking or limited social support and possibility for regeneration in the home environment during the time of crisis. In addition to that, infections with partly complicated progress of disease, of medical personal is not excludable despite of thorough protective measures. Understandably this can lead to emotional distress of the remaining clinical colleagues. However, the challenges perceived in times of crisis can also lead to positive effects like increased collegiality, solidarity and sense of purpose in the conducted occupation.
The aim of this literature overview is to systematically investigate and summarize publications on psychosocial impacts and possible risk factors linked to COVID -19 pandemic. The literature review should identify possible criteria that should contribute to the establishment of concepts for accompanying research as well as the development of multidimensional supply- and (health -) care services, that are adapted to acute emergency situations.
Methodology
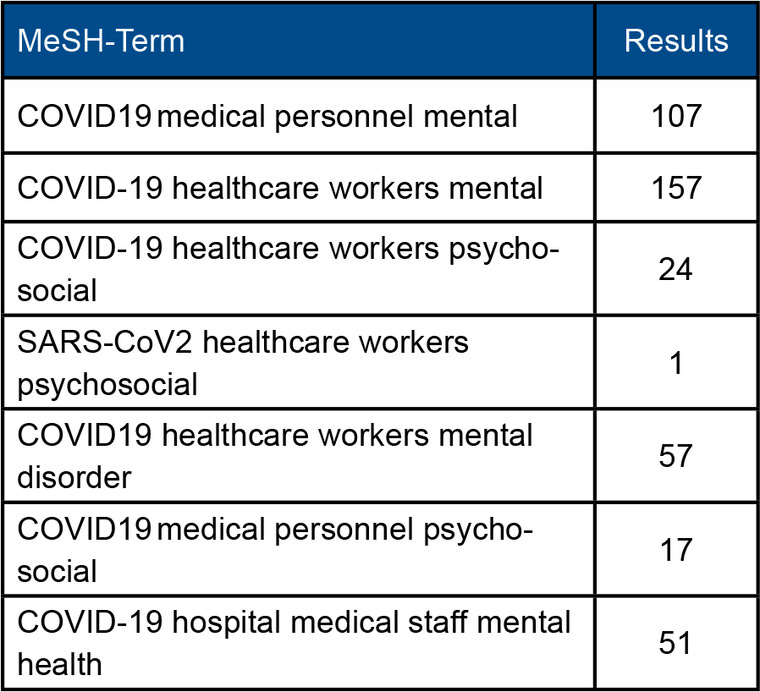
The systematic literature analysis adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12]. PubMed- database was used for literature research. In order to identify relevant studies, that were published between February and June 2020, keyword phrases pertinent to the psychosocial effect of the COVID- 19 pandemic were used. Table 1 shows a full summary of the keyword phrases.
Table 1: MeSH-Terms and number of identified publications
A preliminary assessment of titles and abstracts of the search results was performed, followed by a second stage that involved careful review of the full -text publications. Studies were included if they investigated the psychosocial effects of the COVID-pandemic on people working in the medical sector. The literature search identified 414 articles. Duplications, reviews , comments and editorials were eliminated. The remaining publication underwent full -text analysis and were selected according to the exclusion criteria outlined in figure 1. A summary flowchart of our literature search according to PRISMA guidelines is found in figure 1 . Following the application of the inclusion and exclusion criteria, 29 publications were included in the final analysis. We wanted to find out if i) a specific symptom burden arises pandemic related, ii) what impact COVID-19 exposition has on the symptomatic and iii) if there are social and epidemiological differences .
Results
The included publications were mostly carried out in Asia and were conducted between February and June 2020. A detailed overview of the publications can be found in table 2. The studies almost exclusively investigated short cross-sectional self-assessment online -surveys.
Symptom burden in general
All surveys showed psychological burden for medical staff working during the COVID-19 pandemic. Studies report on anxiety disorders, depressive disorders, insomnia and stress related reactive disorders. The prevalence varied greatly between the studies. DAUGHERTY and ARBLE [1] reported on a total prevalence of 35.4 % for post-traumatic stress disorder, depression, anxiety and general distress. The prevalence for anxiety lay between 12.5-70.6 % (weighted average: 42.37 %) [2][3][5][7][9][12][15][17 ][18][21][27][30]. Depressive symptoms lay between 12.1-64.7 % ( weighted average: 50.7 %) [2][3][5][7-9][15-19][21][27 ][30]. The studies showed a prevalence for insomnia between 8.27-61.67 % (weighted average: 28.99 %) [7][9][12][16][17][21 ][22][25][30]. Sleeping quality seemed to be linked to other psychological symptoms, especially depression [2][12][21][22]. The prevalence of general distress and acute stress disorders was comparatively low with a prevalence of 3.8-9.1 % [19][28]. Unspecific acute stress reactions like arousal and insomnia were more prevalent with prevalence rates of 21.9-73.4 % (weighted average: 54.93 %). Huang et al. showed that medical personal had a worse sleeping quality when compared with other professions like teachers and administrative employees [ 2][3][9][17][18][30].
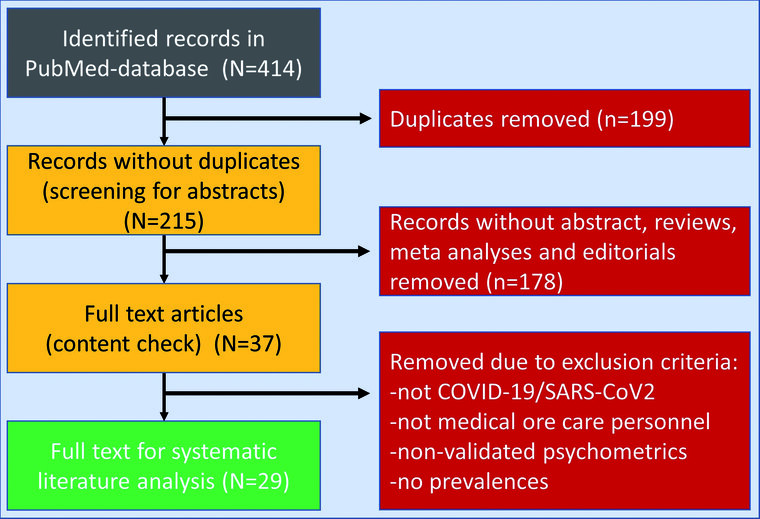
Fig. 1: Flowchart according to PRISMA guidelines for systematic reviews and meta-analyzes (LIBERATI et al., 2012 [12])
Occupation-specific effects
Some of the selected publications performed subgroup analyses of different medical occupational groups. The studies showed that care staff was exposed to higher levels of stress compared to health professionals or administrative employees within the health sector. These findings could also be replicated within European samples. GARCIA-FERNANDEZ et al. [4] demonstrated that care staff showed significantly higher levels of anxiety, depressive symptoms and stress than all other medical professional groups. In a German sample ZERBINI et al. [29] could show that care staff employed on a special COVID-19 ward had a higher symptom burden. This difference was not demonstrable for medical professionals. Higher symptom burden for care staff compared to medical staff was also described in studies from Asia [ 9;19;33]. Similarly, SHECHTER et al. [18]. could also portray higher prevalence of anxiety, depression, stress and insomnia in US-American care staff than medical staff or administrative employees. Explanatory modally explain these findings with the greater workload, work intensity and direct patient contact [26]. Overall people working in the medical sector seem to be exposed to a higher stress experience compared to the general population [15][26][28][32].
Gender-specific effects
A higher burden of stress could be identified for females working in the medical sector consistently. Especially the stress experience with the development of depressive symptoms was more prevalent in females [2][3][8][9][31][32]. ROSSI et al. [17] exhibited a higher risk for anxiety and stress disorders [28], as well as insomnia [10] for female personal.
COVID-19-specific effects
A considerable proportion of the included publications made attempts to explain the psychological impact of the pandemic on people working in the health sector. Overall, the studies showed, that the closer a person worked to the “ front line” of COVID-19-care, the higher the risk for the development of depressive symptoms and anxiety [3][9][ 13][15][16][21][22][25][26][28][29]. QUE et al. [16] demonstrated that the pandemic-associated psychological impact was more pronounced if the respondent was lacking intrinsic motivation and if other family members were also active in COVID- 19-care. Several studies from the Wuhan region [9][10][21] showed an exposure dependent increase of symptom burden, frequently associated with severe sleeping disorders. Similarly, a Turkish publication showed a significant symptom burden increase as due to longer work hours, a high number of COVID-19 cases, limited assistance from supervisors and restricted logistical and material support [3]. In addition to that a significant proportion of the respondents stated that they questioned their own professional competence. LU et al. [15] identified work on an isolation ward, concern of infection, lacking protective equipment, perceived lack of control over the pandemic situation, frustration over work results and social support as influencing factors for stress experience. The study also demonstrated a higher burden of depression and anxiety the closer the medical staff worked with COVID-19 patients. In contrast SUN et al. [20] could not demonstrate any differences in perceived stress. LI et al. [11] even found that highly exposed personal showed a lower PTSD symptom burden. This could be explained by the fact that the mentioned study was conducted in a time where the medical system in Wuhan was no longer overstrained. In addition to that it must be noted that personal from less affected Chinese regions was engaged in hotspot regions like Wuhan in order to replace the overcharged or infected Wuhan care and medical personnel.
Discussion
The presented findings on the psychosocial effects of the COVID-19 pandemic on personal working in the medical sector demonstrated a higher degree of symptom burden for medical personal when compared to the general public. However, the results must be viewed with caution when considering that most of the studies not only originate from the Asiatic region but are regionally restricted. Many of the studies draw their sample from the epicentre China, especially the region Hubei, respectively the city of Wuhan [2][5-11][13-16][ 19-22][25-28][30-33]. The pandemic situation in spring 2020 in this region is probably not comparable with the continuously, overall regulated care situation in the German military hospitals. The prevalence rates of the different psychosocial effects vary greatly between the studies due to the different composition of the investigated samples. Especially the multisite studies demonstrate regional differences in psychosocial effects [ 10][26][32]. In addition to that further research must fcous possible transcultural differences of the pandemic related stress experience. A study that compared a German and Chinese sample showed that the German respondents had lower stress levels than the Chinese respondents, while no gender-related differences could be identified. On the other hand, other studies, suggest that there are gender-related differences in stress experience [23][24], which could be explained by differences in the emotional and cognitive processing between males and females.
European studies [4][16][26] were constant in their results, that demonstrated higher stress levels for medical personal, presented in the form of distress, anxiety and exhaustion. These symptoms were most pronounced in care personnel. Stress level was perceived higher the closer the personnel worked in the COVID- 19 care and supply. Possibly these symptoms are higher in regions where hospitals reach their load limit and supply of material and medication, logistic and therapeutic processes and regeneration of personnel cannot be ensured [15][16][18][19].
The results portrayed in this literature review are limited by the survey methodologies, that were mostly short, self-assessment online surveys. Further it must be noted that the psychosocial situation of the respondents cannot be directly linked to the COVID-19 pandemic, as the examination were all cross-sectional study. In order to minimize this limitation most of the studies had control groups from the general public. Nevertheless, the results must be viewed with caution. In future further long-term studies, that compare different demographic and social traits will be necessary.
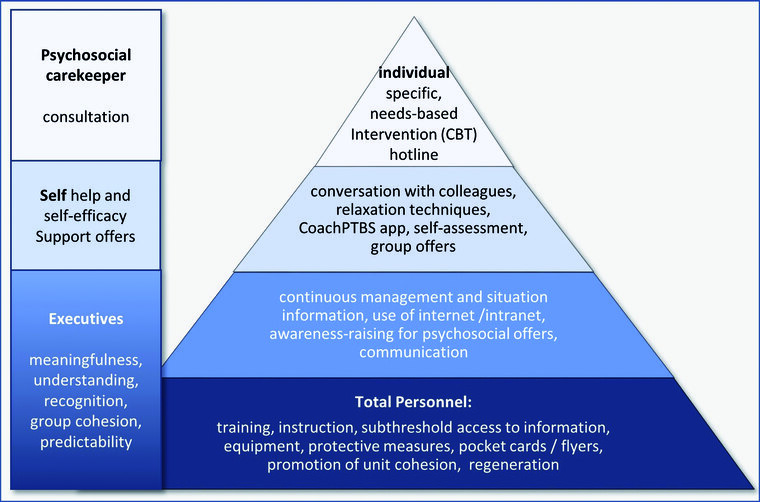
Figure 2: “Care pyramid” for prevention and, if necessary, intervention in the event of psychological stress
Conclusion
Acknowledgement, positive feedback, education and information of personnel and regular updates on the situation and protective equipment have been described as basic measures in the support of employees as they seem to be closely linked to their psychological wellbeing. The German military hospitals introduced a series of measures in order to safeguard the psychosocial wellbeing of its employees. For example, the Military Hospital Berlin set up, low-threshold information portals in its internal communication network of the hospital information system. In addition to that short videos were produced the commanding officer that gave an overview on the current situation. Similarly, tutorial videos for hygiene training and relaxation exercises were produced and provided for employees . Finally, a holistic, integrative and multiprofessional psychosocial support concept was established for local staff. The medical service of the German Armed Forces however also provides singular low-threshold psychosocial care possibilities with its social and psychological services and military chaplaincy as well as military GPs, psychiatric, psychotherapeutic offers. The COVID -19 pandemic has shown that these counselling and therapeutic offers should be complemented and enhanced for example in the form of online consultation sessions in order to provide and ensure a seamless and secure patient care. The literature review has also shown that medical personnel was concerned about the wellbeing of relatives and family members. Especially the lockdown in many countries has demonstrated how supervision bottlenecks can negatively affect the working environment in the hospital. In future executives on all levels will have to display understanding and elaborate manageable solutions so that family and social support, being important psycho-protective elements, are effective.
References
- Daugherty AM, Arble EP: Prevalence of mental health symptoms in residential healthcare workers in Michigan during the covid-19 pandemic. Psychiatry Res 2020; 291: 113266. mehr lesen
- Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, Liu B, Zhang M, Yin Y, Qin J, Bouey J, Zhao M, Li X. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry 2020: S0163-8343(20)30045-1. mehr lesen
- Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E: Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemic. Psychiatry Res 2020; 290: 113130. mehr lesen
- García-Fernández L, Romero-Ferreiro V, López-Roldán PD, Padilla S, Calero-Sierra I, Monzó-García M, Pérez-Martín J, Rodriguez-Jimenez R: Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol Med 2020; 27: 1-3. mehr lesen
- Guo X, Wu L, Yu X, Sun Z, Liu W: Mental Health Care for Military Personnel in the COVID-19 Epidemic. Mil Med 2020: usaa127. mehr lesen
- Hou T, Zhang T, Cai W, Song X, Chen A, Deng G, Ni C: Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS ONE 2020; 15(5): e0233831. mehr lesen
- Huang Y, Zhao N: Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020; 288: 112954. mehr lesen
- Kang L, Ma S, Chen Met al.: Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun 2020; 87: 11-17. mehr lesen
- Lai J, Ma S, Wang Y al.: Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. .JAMA Netw Open 2020; 3(3): e203976. mehr lesen
- Li Z, Ge J, Yang M, Feng J et al.: Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun 2020; 88: 916-919. mehr lesen
- Li X, Yu H, Bian G et al.: Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav Immun 2020; 87: 140-141. mehr lesen
- Liberati A, Altman DG, Tetzlaff J et al.: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6(7): e1000100. mehr lesen
- Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, Cheng ASK: The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology and Infection 2020; 148: e98, 1–7. mehr lesen
- Liu S, Heinz A: Cross-Cultural Validity of Psychological Distress Measurement During the Coronavirus Pandemic. Pharmacopsychiatry 2020: 10.1055/a-1190-5029. mehr lesen
- Lu W, Wang H, Lin Y, Li L: Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res 2020; 288: 112936. mehr lesen
- Que J, Shi L, Deng J, Liu J et al.: Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020; 33(3): e100259. mehr lesen
- Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, Rossi A: Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open 2020; 3(5): e2010185. mehr lesen
- Shechter A, Diaz F, Moise N et al.: Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 2020; 66: 1-8. mehr lesen
- Song X, Fu W, Liu X et al.: Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun 2020; 88: 60-65. mehr lesen
- Sun D, Yang D, Li Y et al.: Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol Infect 2020; 148: e96. mehr lesen
- Tu ZH, He JW, Zhou N: Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine (Baltimore) 2020; 99(26): e20769. mehr lesen
- Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D: Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med (Lond) 2020; 70(5): 364-369. mehr lesen
- Wesemann U, Zimmermann P, Bühler A, Willmund GD: Gender Differences in Hostility and Aggression Among Military Healthcare Personnel After Deployment. J Womens Health (Larchmt) 2017; 26(10): 1138. mehr lesen
- Wesemann U, Zimmermann PL, Mahnke M, Butler O, Polk S, Willmund G: Burdens on emergency responders after a terrorist attack in Berlin. Occup Med (Lond) 2018; 68(1): 60-63. mehr lesen
- Wu K, Wei X: Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med Sci Monit Basic Res 2020; 26: e924085. mehr lesen
- Wu W, Zhang Y, Wang P et al.: Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy J Med Virol. 2020; 10.1002/jmv.25914. mehr lesen
- Yang S, Kwak SG, Ko EJ, Chang MC: The Mental Health Burden of the COVID-19 Pandemic on Physical Therapists. Int J Environ Res Public Health 2020; 17(10): 3723. mehr lesen
- Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, Shang Z, Zhou Y, Liu W: Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother 2020; 27(3): 384-395. mehr lesen
- Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H: Psychosocial burden of healthcare professionals in times of COVID-19 - a survey conducted at the University Hospital Augsburg. Ger Med Sci 2020; 18: Doc05. mehr lesen
- Zhang C, Yang L, Liu S et al.: Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontm Psychiatry 2020; 11: 306. mehr lesen
- Zhang SX, Liu J, Afshar Jahanshahi A, Nawaser K, Yousefi A, Li J, Sun S. At the height of the storm: Healthcare staff's health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav Immun 2020; 87: 144-146. mehr lesen
- Zhu J, Sun L, Zhang L et al.: Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front Psychiatry 2020; 11: 386. mehr lesen
- Zhu Z, Liu Q, Jiang X, Manandhar U et al.: The psychological status of people affected by the COVID-19 outbreak in China. J Psychiatr Res 2020; 129: 1-7. mehr lesen
Manuscript data
Submitted: 10 July 2020
Accepted: 10 August 2020
Citation
Willmund GD, Youssef Y, Helms C, Buehler A, Zimmermann P, Wesemann U: Psychosocial impact on medical personnel fighting the Corona pandemic – a systematic literature review. WMM 2020; 64(9): e27.
For the authors
Colonel (MC) Dr. Gerd-Dieter Willmund, Oberstarzt
Bundeswehr Hospital Berlin
Bundeswehr Psychotrauma Centre
Scharnhorstrasse 13, D-10115 Berlin
Annex
Table 2: Research on the mental health of medical personnel
|
Authors |
Region |
Sample |
Tests |
Summary of results |
|
Daugherty AM & Arble EP, 2020 [1] |
US |
n=113 HCW |
PCL-5 DASS |
The overall prevalence for PTSD, depression, anxiety disorders, or distress was 35.4%. Age, profession and gender had no influence. Social support in the professional as well as in the family environment had a protective effect. Changes in occupational tasks increased the symptoms. |
|
Du J et al., 2020 [2] |
CHN, 02/2020 |
n=144 HCW cross-sectional online-survey |
PSS BDI-II BAI |
Prevalence: 12.7% of HCW at least symptoms of mild depression or 20.1% symptoms of anxiety. 59.0% had moderate to severe perceived stress. This occurred more frequently with female staff, local, highly exposed staff, with poorer training, with a lack of psychological support, a lack of self-efficacy, a lack of family support and poor sleep quality. Anxiety symptoms also occurred more frequently in the event of increased stress, a lack of knowledge about COVID-19, a higher level of education or infections in family and friends. |
|
Elbay RY et al., 2020 [3] |
TUR |
n=442 HCW |
DAS-21 |
Prevalence: 64.7% of HCW showed symptoms of depression, 51.6% anxiety and 41.2% stress. RF: placed in the front line, female gender, young age or single relationship status. Frontline work was associated with higher weekly working hours, higher numbers of COVID19 patients cared for, lower support from peers and supervisors, lower logistical support, and lower COVID-19-associated expertise. |
|
García-Fernández L et al., 2020 [4] |
ESP |
n=1786 cross-sectional online-survey |
HARS ASDI |
HCW with higher symptom burden of acute stress than non-HCW, anxiety and depression showed no significant group differences. Nursing staff showed significantly higher levels of exposure in all dimensions than other HCW subgroups. The burden loads were more pronounced in the infected HCW in all dimensions than in the non-infected HCW. Satisfaction with information and availability of protective equipment correlate with emotional well-being. |
|
Guo X et al., 2020 [5] |
CHN |
n=642 HCW military |
PHQ-9 |
Special feature: military sample, medical service (CHN) Prevalence (anxiety symptoms): 29.44%, Prevalence (depression): 36.45%. RF (anxiety and depression): existing concerns about being infected with COVID-19 in own family. |
|
Hou T et al., 2020 [6] |
CHN 02/2020 |
n=1472 HCW |
SSRS CD-RISC SCL-90 |
Special feature: investigation focussed on resilience and protective factor of social support Resilience acts as a mediator of the effects of social support on the mental health of HCW. The age group moderated the indirect relationship between social support and mental health through resilience. In particular, when compared to younger healthcare workers, the relationship between resilience and mental health would be weakened in middle-aged workers. |
|
Huang Y, Zhao N, 2020 [7] |
CHN 02/2020 |
n=7236 |
SDS |
Prevalence (sleep disorder): 23.6% of HCW (significantly more than other professions). Work intensity, longer working hours, less regeneration were associated with it. Prevalence (depression and anxiety symptoms): 20.1% or 35.6% of HCW (no significant difference to other non-HCW professions (teachers, students, employees) |
|
Kang L et al., 2020 [8] |
CHN |
n=994 HCW cross-sectional online-Survey |
PHQ-9 |
Prevalence (depression): mild 34.4% of HCW, moderate 22.4%, severe 6.2%. Female HCW were affected significantly more often. |
|
Lai J 2020 et al. 2020 [9] |
CHN |
n=1257 HCW |
PHQ-9 IES-R |
Prevalence: depression 50.4%, anxiety 44.6%. Insomnia 34.0%, distress 71.5%. Nurses, women and frontline staff and those in the Wuhan epicenter had a significantly higher symptom burden in all disease dimensions. |
|
Li Z et al., 2020 [11] |
CHN 02/2020 |
n=740 |
VTQ |
COVID caregivers showed lower levels of PTSD exposure than „non-COVID“ caregivers or the general population. There were no significant differences between non-frontline HCW and the general population. |
|
Li X et al., 2020 [10] |
CHN 02/2020 |
n=948 HCW |
AIS |
Special feature: Investigation of two regions that were affected to different degrees. Prevalence (sleep disorders): Wuhan group 58.90% vs. Ningbo group 24.97% (p = 0.001) and had a higher prevalence (overall psychological burden): Wuhan group 13.24% vs. Ningbo group 8.64 (p = 0.044) Insomnia was associated with women, higher levels of psychological symptoms, and low educational attainment. |
|
Liu CY et al., 2020 [13] |
CHN 02/2020 |
n=512 HCW |
SAS |
Prevalence (anxiety disorders): 12.5% of HCW. After adjusting for socio-demographic characteristics (gender, age, education and marital status), medical staff who had direct contact to treat infected patients achieved higher levels of anxiety than staff who had no direct contact (β value = 2.33, CI 0.65-4.00 ; P = 0.0068). A similar trend was observed among healthcare workers from Hubei Province compared to HCWs from other parts of China (β value = 3.67, CI 1.44–5.89; P = 0.0013). COVID-19 suspected cases achieved higher anxiety scores compared to non-suspicious cases (β value = 4.44, CI 1.55–7.33; P = 0.0028). |
|
Lu W et al., 2020 [15] |
CHN |
n=2299 HCW |
NRS HAMD |
Prevalence (anxiety symptoms): 70.6% of the medical vs. 58.4% of the administrative staff complained (p <0.001). Prevalence (depression): 12.1% of the medical staff RF (distress): work in the isolation ward (p <0.001), worrying about one‘s own infection (p <0.001), lack of protective equipment (p <0.001), lack of control over the pandemic (p = 0.002), frustration with unsatisfactory Work results (p <0.001), lack of social support (p = 0.005). The closer the staff was exposed to COVID-19 patients, the higher the risk of experiencing anxiety and depressive symptoms than with non-curative staff (OR 2.062; 95%). |
|
Que J et al., 2020 [16] |
CHN |
n=2285 HCW |
GAD-7 ISI |
Prevalence: anxiety symptoms 46.04%, depression 44.37% and sleep disorders 28.75%. The more directly in contact with COVID19 patients, the greater the burden of symptoms for anxiety and depression. RF (anxiety, depression): negative feedback / information, little intrinsic willingness to work with maximum exposure, family members in “frontline” work |
|
Rossi R, et al., 2020 [17] |
ITA |
n=1379 HCW cross-sectional online-survey |
GPS |
Prevalence: 49.38% PTSD, 24.73% depressive symptoms, 19.80% anxiety symptoms, 8.27% insomnia, 21.90% distress. Female HCWs were at higher risk for anxiety symptoms, stress disorder, and depression. Being on the front line has been associated with stress disorder. RF (distress): Illness, death or quarantine of colleagues. |
|
Shechter A et al., 2020 [18] |
US 04/2020 |
n=657 HCW |
PC-PTSD |
Prevalence: acute stress in 57%, depression 48% and anxiety symptoms 33%. Nursing staff show a higher burden of symptoms (stress, depression and anxiety) than doctors or administrative employees. Coping strategies 59% through physical training. 33% were interested in online counseling by therapists. Prevalence (sleep disorders): 45%, the proportion of nurses was significantly higher. Distress was mainly associated with a feeling of loss of control, fear of transmission of COVID19 into one‘s own family, concern for the health of relatives, but also the experience of structural deficits such as a lack of tests and protective equipment. |
|
Song X et al., 2020 [19] |
CHN 02-03/2020 |
n=14825 HCW cross-sectional online-survey |
PCL-5 |
Special feature: later survey time (fall of the first pandemic wave), possibly lower prevalence 31 provinces in CHN were examined. Prevalence for PTSD 9.1%, depressive symptoms 25.2%. RF (PTSD): mean. Age, few years of service, high daily working hours, lower social support, employed in Hubei. Nurses show higher risk of PTSD. Male Gender is associated with higher risks for PTSD and depression. |
|
Sun D et al., 2020 [20] |
CHN |
n=442 HCW cross-sectional online-survey |
IES |
No gender-specific differences in arousal. Minor effects on the staff. |
|
Tu ZH et al., 2020 [21] |
CHN |
n=100 HCW |
PSQI |
Special feature: exclusively female nursing staff from Wuhan / CHN Prevalence (sleep disorders): 76%, especially disorders of sleeping through the night (DMS) or early awakening (EMA). 45% complained of nightmares. 19% of the staff studied used hypnotics during exposure to COVID-19. Prevalence (depression): 46% of HCW, Prevalence (anxiety disorder): 40% of HCW. Sleep quality and symptoms of anxiety were associated with symptoms of depression. Growing up as an only child was associated with a higher burden of depressive symptoms. Depression symptoms were associated with poor sleep quality. The front line work also resulted in a significantly higher symptom burden compared to other Chinese regions. |
|
Wang S et al., 2020 [22] |
CHN |
n=123 HCW cross-sectional online-survey |
PSQI SAS SDS |
The prevalence of sleep disorders was 38%, the occurrence of which was associated with symptoms of anxiety and depression. RF (sleep disorders): only child status, contact with COVID-19 patients and symptoms of depression; the connection with anxiety symptoms could not be proven. |
|
Wu K & Wei X, 2020 [25] |
CHN |
n=120 |
SCL90-R |
Somatization, depression, and anxiety were higher than normal in the medical staff exposed to COVID-19. Symptoms of stress and depression were present to a greater extent in the test group than in the normal, non-exposed control group (P <0.05). In addition, the test group showed poorer sleep quality. The prevalence for moderate insomnia was 61.67% (severe insomnia 26.67%). |
|
Wu W et al., 2020 [26] |
CHN 02-03/2020 |
n=4268 |
In all regions in China, medical personnel showed higher exposure severity than a student control group; Wuhan group showed significantly higher fears of their own infection or infection of the family (p <0.05), poor sleep quality, need for psycholog. Support, annoyance about own infection (p = <0.01). Indications of exposure effect. |
|
|
Yang S et al., 2020 [27] |
KOR |
n=65 HCW -PT cross-sectional online-survey |
PHQ-9 |
revalence of anxiety symptoms and depression 32.3% and 18.5%, respectively. RF: Anxiety symptoms were more common when the people were parents of small children, depression was more common in people in the 30-39 or 50-59 age group. |
|
Yin Q et al., 2020 [28] |
CHN |
n=377 HCW |
PCL-5 PSQI |
The prevalence of PTSD was 3.8%. Female medical staff were significantly more affected. HCW with higher exposure levels also rated significantly more hyperarousal. There was a significant difference in sleep quality between participants with and without PTSD and between different groups with different contact frequencies |
|
Zerbini G et al., 2020 [29] |
DEU |
n=110 HCW |
PHQ |
Significantly higher experience of stress, fatigue, depressive mood in COVID-19 ward nursing staff compared to normal ward nursing staff; there was no difference in medical staff. |
|
Zhang C et al., 2020 [30] |
CHN |
n=1563 cross-sectional online-survey |
ISI |
Prevalence of symptoms of depression, anxiety and stress was 50.7%, 44.7%, 73.4% The prevalence of sleep disorders was 36.1%, associated factors were low level of education, medical profession, work in isolation ward, fears about personal risk of infection, uncertainty about how to control the pandemic situation |
|
Zhang SX et al., 2020 [31] |
IRN 04/2020 |
n=304 HCW cross-sectional |
SF-12 PHQ-4 K6 |
Prevalence of stress symptoms 20.1%, depression 20.6% and anxiety 28.0%. Female staff significantly more susceptible to distress and depression. COVID-19 positive staff more affected by distress, depression and anxiety. Age correlates negatively with mental but positively with physical symptom burden. |
|
Zhu Z et al., 2020 [32] |
CHN |
n=922 |
SCL90 |
2 recruiting times; 71% medical. Staff. Stress severity was lower in the second recruitment. Wuhan has higher stress levels. Medical personnel have a higher burden. 18.3% psych. Burden. RF: female Gender; does stress decrease after epiphase? |
|
Zhu J et al., 2020 [33] |
CHN 02/2020 |
N=155 |
SDS SCSQ |
Prevalence (doctors n = 79): anxiety symptoms 11.4%, depressive symptoms 45.6% RF (fear): previous psych. Erkr., Female Closed Prevalence (nurses n = 86): Anxiety symptoms 27.9% Depressive symptoms: 43.0% RF (depression): previous mental illnesses |
|
List of abbreviations |
||||
|
Region |
CHN China, DEU Germany, ESP Spain, KOR South Korea, ITA Italy, USA United States of America |
|||
|
Sample |
HCW Healthcare Worker |
|||
|
Psychometrics |
AISDI Acute Stress Disorder Inventory, AIS Athens Insomnia Scale. BAI Beck Anxiety Inventory (BAI), BDI Beck Depression Inventory, CES-D Center for Epidemiologic Studies Depression Scale, CD-RISC, Connor-Davidson Resilience scale, DASS Depression Anxiety Stress Scale; GAD-2 General Anxiety Disorder 2 Items, GAD-7 General Anxiety Disorder 7 Items, GPS Global Psychotrauma Screen, HAMA Hamilton Anxiety Scale, HAMD Hamilton Depression Scale, IES Impact of Event Scale, ISI Insomnia Symtoms Inventory K6 K-6 Distress Scale, LOT-R Life Orientation Test revised, MBI Maslach Burnout Inventory, NRS Numeric Rating Scale, PC-PTSD Primary Care PTSD, PCL-C Posttraumatic Stress Disorder Checklist for DSM-5 civil, PHQ Patient Heath Questionnaire, PSQI Pittsburgh Sleep Quality Index, PSS Perceived Stress Scale SAS self-rating anxiety scale, SCSQ simplified coping style questionnaire, SCL90 Symptom Checklist 90, SCL90-R Symptom Checklist 90 revised, SDS self-rating depression scale, SF-12 Short Form Survey 12 Items, SRQ-20 Self-Reporting Questionnaire-20, SSRS Social Support Rating Scale, VTQ Vicarious Traumatization Questionnaire |
|||
|
Results |
CI confidence interval, RF risk factors, OR odds ratio |
|||