Exertional overheating in the civilian and military sector – an underestimated hazard
Karl Jochen Glitza , Alexander Sieverta , Ulrich Rohdea , Claus Piekarskib , Dieter Leyka, c
a Bundeswehr Institute for Preventive Medicine
b University of Cologne, Institute and Policlinic for Occupational Medicine, Environmental Medicine and Prevention Research
c German Sport University Cologne, Research Group Performance Epidemiology
Introduction
The human heat balance is largely dependent on physical workload, clothing insulation , ambient climate and individual factors (degree of acclimatisation, physical performance capabilities, etc.).
There is a risk of exertional overheating if heat generated by working muscles cannot be sufficiently dissipated. This threat is often underestimated or not even recognised [13]. When heat cramps, heat syncopes or heat exhaustion are diagnosed, these clinical pictures are often seen as non-critical, although they may unexpectedly and rapidly evolve into life-threatening, exertional heat stroke (EHS). In this case, effective first aid measures must immediately be initiated. Otherwise, valuable time to prevent generalised endothelial cell damage in various organ systems, and subsequent multiorgan failure due to systemic inflammatory reactions (SIRS) is irretrievably lost [7][11].
Examples of exertional heat stress
Exertional overheating often occurs during top level sports performance in hot climates (e. g. Road World Cycling Championships in Qatar 2016). However, it is hardly known that these clinical pictures also emerge in moderate climates during long periods of hard physical work: During the 2018 London Marathon, athletes collapsed due to high metabolic heat production in the working muscles because they were unable to maintain their heat balance at ambient temperatures of 23 ° C.
In the occupational sector, this risk may be mitigated by preventive measures from occupational medicine and by work organisation. Nevertheless, there are reports of heat incidents caused by misjudgements ( e.g. heavy agricultural work in the summer heat).
The characteristics of military occupations (strenuous physical work, high heat insulation caused by body armor, deployments in hot climates, lack of acclimatisation due to rapid climate zone changes, dehydration, long exposure times, sleep deprivation, and many more) result in a high risk of exertional heat illness. Recent reports from the US Armed Forces (2020: 475 incident cases of heat stroke and 1,667 incident cases of heat exhaustion [1]) underscore the necessity for action regardless of nation. However, recommendations for the prevention of heat illness from the civilian sector such as limiting shift duration and regulating work organisation options are of limited applicability in armed forces. Therefore, NATO has climate prevention recommendations that are adapted to military conditions [12].
Diagnosis and first aid for exertional heat stroke
The diagnosis of exertional heat stroke requires reliable recording of the core body temperature by rectal measurements. The longer core body temperatures remain above 40.0 °C, the worse the prognosis. Immediate, effective full-body cooling is the causal therapy for exertional heat stroke [7][11]. The narrow time frame to do so is about 30 min. Therefore, cooling to rectal temperatures below 39.0 °C , better to 38.5–38.0 °C, must take place before transport to clinical care [4].
Promising cooling rates of 0.2–0.35 °C/min are achievable by cold or ice water immersion (full bath) only (Fig. 1). Although this drastic “physical” measure significantly reduces blood flow in and to the body surface due to a reflex vasoconstriction of the peripheral blood vessels , it provides effective, predominantly conductive heat dissipation of the entire body. Ideal, as in “physiologically controlled”, cooling measures with simultaneous monitoring of skin temperature to control blood flow, combined with rectal temperature measurement to ensure therapeutic success, are not feasible during prehospital care.
If no other means of cooling are available during the initial care phase, sufficient wetting of the body surface must at minimum be ensured to support evaporative heat dissipation before and during transport.
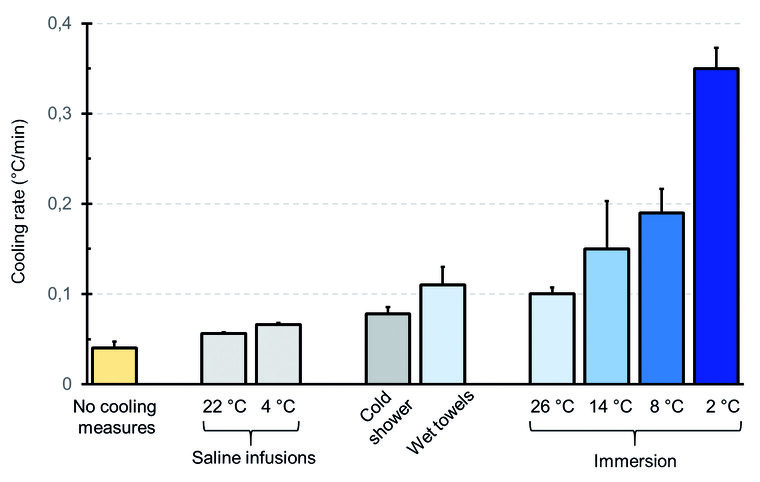
Fig. 1: Quick overview of cooling rates of the human body using different cooling methods. The total volume of the 0.9 % saline infusions were 2 l each. Cooling rates of 0.2–0.35 °C/min are only achieved using cold or ice water immersion. (Source: Evaluation of various studies that are not standardised among each other (modified after Leyk et al. 2019 [11]; reprinted with kind permission of the Deutsche Ärzteblatt International))
Prevention of exertional heat illnesses
The pivotal element for the prevention of exertional heat illnesses is the risk assessment during the preparation phase of planned projects (sporting events, commercial ventures, military training measures, etc.):
One prerequisite is the assessment of ambient climate using a valid climate index that allows for the assessment of the effects of the four climate parameters (air temperature, humidity, wind speed and thermal radiation) on the human body. One common measure is the Wet Bulb Globe Temperature , WBGT [3][12] which is often reported in weather forecasts . In addition, the local current weather situation can be independently assessed with market-available WBGT measuring devices (Fig. 2).

Fig. 2: Example of a commercially available climate measuring device that can be used to determine the Wet Bulb Globe Temperature (WBGT) as a climate index to assess the local current conditions.
Climate adapted measures
If the climatic situation is known, tailored preventive measures can be taken. The Bundeswehr follows the medical recommendations of NATO [12] to estimate possible workloads , adequate working time/ rest regimes and the required fluid intake for the respective heat categories, while accounting for effects of clothing insulation (Fig. 3). If excessive heat stress is to be expected, a decision whether to postpone planned activities to cooler times of day or to cancel them must be made.
Comprehensive heat prevention required
Comprehensive heat prevention can only be successful if everyone involved is aware of the dangers of exertional overheating . In sports, this includes all involved from the organiser to the individual athlete. Comparable recommendations exist for risk assessment leading up to a planned event [2]. Respectively, everyone from company management, occupational healthcare service to the individual employee, are required to implement and follow heat stress prevention measures [5].
In case of the Bundeswehr, intensifying the approach taken by providing information on preventive heat stress management on all levels, including (first aid) training and the provision of a quick reference card for all personnel is recommended [6]. This pocket guide was developed under the central coordination of the Bundeswehr Institute for Preventive Medicine (InstPrävMedBw) and describes the most important factors in the development of heat stress, the recognition of exertional heat illnesses and applicable first aid measures [9][10]. Instructors of particularly exposed training units were sensitised and trained in the action guidelines of an extended pocket guide version (Figure 3) for trainers in a pilot project. The flyer “Hot Ten”, issued by the InstPrävMedBw was also used as for training the trainers [8].
In view of reoccurring summer heat waves in Germany and the Bundeswehr’s worldwide deployments in hot climates, it is foreseeable that the importance of preventing exertional heat illnesses in the civilian and military sectors will increase even further.
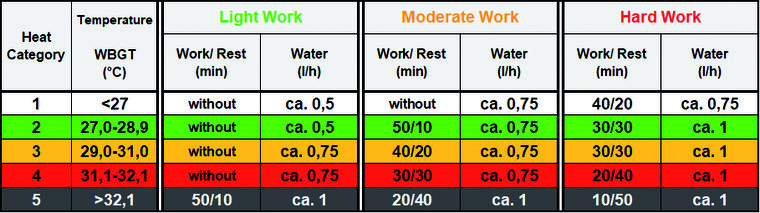
Fig. 3: Extract from the extended pocket guide “Working without overheating” for instructors, which was developed under the central coordination of the Bundeswehr Institute for Preventive Medicine (InstPrävMedBw) as part of a pilot project. Recommendations are intended for heat-acclimatised personnel wearing standard field uniform. The table (modified according to [12]) allows an estimation of possible workloads, adequate working time/ rest regimes and required fluid intake in the respective heat categories (WBGT). If additional clothing insulation is worn, WBGT base values have to be modified accordingly (e.g.: combat helmet +1.5 °C; ballistic vest +3 °C).
References
- Armed Forces Health Surveillance Division: Update: Heat Illness, Active Component, U.S. Armed Forces, 2020. MSMR 2021; 28 (4): 10-15. mehr lesen
- Armstrong EL, Casa JD, Millard-Stafford M et al.: Exertional heat illness during training and competition. ACSM, American College of Sports Medicine (ed.). Position Stand. Med Sci Sports Exerc 2007; 39 (3): 556-572. mehr lesen
- DIN EN ISO 7243:2017-12: Ergonomics of the thermal environment - Assessment of heat stress using the WBGT (wet bulb globe temperature) index. Berlin: Beuth Verlag GmbH mehr lesen
- Epstein Y, Yanovich R: Heatstroke. N Engl J Med 2019; 380 (25): 2449-2459. mehr lesen
- Glitz KJ, Gorges W, Leyk D, Piekarski C: Arbeit unter klimatischer Belastung: Hitze. LEITLINIE. [Working under climatic conditions: heat. GUIDELINE] In: Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V. (Hrsg.): Leitlinien der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V.; AWMF online - Das Portal der wissenschaftlichen Medizin 2012 [Guidelines of the German Society for Occupational and Environmental Medicine; AWMF online] (Note: The guideline is currently being updated by four professional societies with the involvement of the Bundeswehr Institute for Preventive Medicine.) mehr lesen
- Glitz KJ, Rohde U, Piekarski C, Leyk D: Prävention bei anstrengungsbedingtem Hitzestress [Prevention of exertion-related heat stress]. Wehrmed Mschr 2020; 64 (1): 42-43. mehr lesen
- Hoitz J: Klinisches Management beim anstrengungsbedingten Hitzschlag [Clinical management in exertion-related heat stroke]. Wehrmed Mschr 2018; 62 (10): 357–359. mehr lesen
- Institut für Präventivmedizin der Bundeswehr (Hrsg.): Flyer: Hot Ten. Infos und Tipps für die Hitze [Flyer: Hot ten. Info and tips for the heat]. Koblenz: InstPrävMedBw.
- Kommando Sanitätsdienst der Bundeswehr BGM (Hrsg.): ARD-874/0-4004a: Arbeiten ohne Überhitzen [General military regulation ARD-874/0-4004a: Work without overheating]. 2018.
- Kommando Sanitätsdienst der Bundeswehr (Hrsg.): ARD-874/0-4004b: Erste Hilfe in der Bundeswehr [General military regulation ARD-874/0-4004b: First aid in the German Armed Forces]. 2019.
- Leyk D, Hoitz J, Becker C, Glitz KJ, Nestler K, Piekarski C: Health risks and interventions in exertional heat stress. Dtsch Arztebl Int 2019; 116: 537–544. mehr lesen
- North Atlantic Treaty Organizsation (ed.): TR-HFM-187: Management of heat and cold stress. Guidance to NATO medical personnel. Findings of Task Group HFM-187. Neuilly-Sur-Seine Cedex: NATO Science & Technology Organization. mehr lesen
- Stacey MJ, Brett S, Woods D, Jackson S, Ross D: Case ascertainment of heat illness in the British Army. Evidence of under-reporting from analysis of Medical and Command notifications, 2009-2013. J R Army Med Corps 2016; 162(6): 428-433. mehr lesen
For the Authors
Dr. Karl Jochen Glitz
Bundeswehr Institute for Preventive Medicine
Department A4 – Environmental Ergonomics
and Clothing
Andernacher Str. 100, DE-56070 Koblenz
E-Mail: karljochenglitz@bundeswehr.org