Optimisation and incentive options for health behavior and individual operational readiness
Kristina Küpera, Sarah Schramma, Alexander Witzkia, Dieter Leyka,b
a Bundeswehr Institute for Preventive Medicine, Andernach, Germany
b German Sport University Cologne, Research Group Epidemiology of Performance, Cologne, Germany
Background
Human health behavior often seems irrational: although the benefits of a healthy lifestyle are well known, for example, only about one third of the EU population achieves 150 minutes of moderately strenuous endurance activity per week as recommended by the World Health Organization [10]. In addition to physical inactivity, excessive alcohol consumption, smoking and unhealthy eating habits are also widespread in the population [16]. Negative consequences of this unhealthy lifestyle are performance deficits, an increased tendency towards overweight and obesity, and an increased risk of various non -communicable diseases, such as cardiovascular disease, type II diabetes and certain types of cancer [2][13].
This societal trend also has consequences for the Bundeswehr: The “General Check-up for Aptitude – Individual Basic Capabilities” ( AVU-IGF ), introduced on January 1st, 2019, shows that, already in middle age, a considerable proportion of soldiers has health problems of such magnitude that they are deemed unable to participate in the yearly tests of basic military capabilities and physical fitness [11]. Of the 40- to 49-year-old soldiers, only about 75 % are sufficiently healthy, in the age group of the over- 50-year-olds less than 40 % are [11].
Soldiers are obligated to take part in sports on duty (“Dienstsport”)[1]. In addition, as part of the corporate health management program, all Bundeswehr personnel have access to a wide range of health promotion services designed to initiate and/ or support lifestyle changes. These include nutrition and exercise programs, smoking cessation seminars and stress management courses, for example. The current AVU-IGF results illustrate, however, that these existing behavioral preventive measures are not sufficient, especially against the background of demographic change.
Behavioral Economics
Outside of the Bundeswehr, behavioral prevention measures are often ineffective because they are underused and do not reach the intended target group [6]. People with unhealthy lifestyles rarely make use of prevention offers [12], even though they stand to benefit the most from them [3]. In addition, what is lacking is often not the willingness to change, but rather perseverance: for most people it is difficult to achieve lasting health behavior changes. This is due to habits, decision- making heuristics, and perceptual distortions, which are the subject of research in behavioral economics, among others. Behavioral economics combines findings from psychology and economics to identify rationales in seemingly irrational behavior.
A core thesis of behavioral economics is that people make decisions not only based on rational cost-benefit considerations, but rather on estimations regarding the probability of events occurring [ 9]. In this, they prefer guaranteed gains and avoid guaranteed losses. Against this background, it becomes clear why lifestyle changes are so difficult to achieve: They represent the guaranteed immediate loss of familiar but unhealthy lifestyle habits in exchange for a merely potential future gain of health and additional life years (see Figure 1).
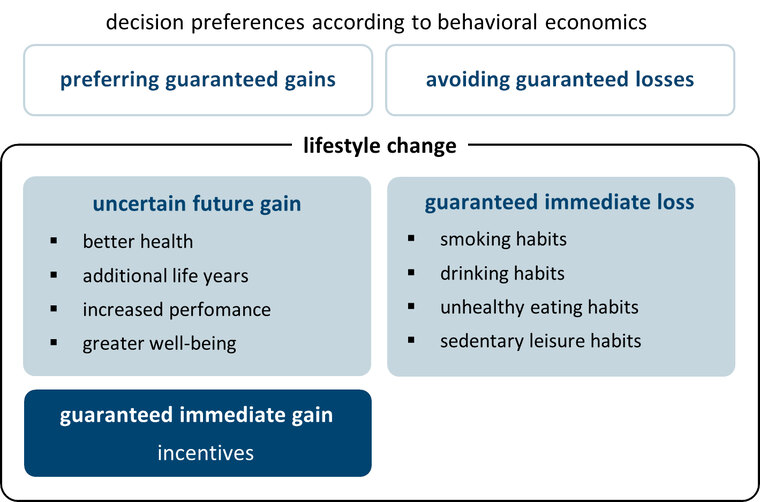
Fig.1: According to behavioral economics, sustainable lifestyle changes are difficult to realize because they run counter to human decision-making preferences: An uncertain future gain cannot compensate for the guaranteed immediate loss of familiar habits. Incentives are effective because they link lifestyle changes to a guaranteed immediate gain.
Incentive programmes
To offset this imbalance, incentives are increasingly used in the field of behavioral prevention. Incentives link lifestyle changes to a guaranteed immediate gain and thus facilitate them (see Figure 1). An example of this are the bonus programs of the statutory health insurance funds, which offer non-cash prizes, vouchers, or refunds as incentives for participating in behavioral prevention measures, such as sports courses. These bonus programs are effective: Those who collect bonus points use behavioral prevention offers more frequently and as a result generate significantly fewer sickness costs [7][15].
The Bundeswehr also already uses incentives, such as medals and special pay, to compensate for difficult service conditions or reward special achievements, for example . So far, however, there is no incentive program focused on health behavior and operational readiness. Based on a selective literature research, the Bundeswehr Institute for Preventive Medicine (InstPraevMedBw) examined whether incentives are suitable for improving individual operational readiness within the Bundeswehr. A particular focus was on identifying weak points of existing incentive systems in order to be able to circumvent them in the conception of a potential Bundeswehr incentive concept for operational readiness.
Although the bonus programs of the statutory health insurance funds are effective, they also show deadweight effects [8]. That is to say that some participants of bonus programs are already health-conscious to begin with and are thus being rewarded for something they would have done anyway . Such deadweight effects underline the importance of a target-group -specific design for the effectiveness of incentive systems. In the military context, different types of soldier motivation must be considerd when selecting possible incentive options, for instance. Existing incentive systems in the Bundeswehr use (1) social recognition (medals, career benefits etc.), (2) compensatory time off (e.g., special leave) or (3) material benefits (special pay, non-cash prizes etc.) as incentives. As rank groups differ in terms of their need orientation [4], the effectiveness of these incentive options will also vary across rank groups, for example.
Establishing norms
Incentives cannot substitute for intrinsic motivation. Thus, some behavioral changes achieved with the help of incentives only persist until the incentives are removed [14]. Incentives should therefore be used primarily to initiate behavioral changes. Additional measures are required to consolidate these behavioral changes, for example in terms of establishing healthier habits. Particularly anchoring can be helpful in this respect, i.e., the fact that behavior is strongly influenced by reference values [ 5]. Such reference values can be social norms, for example: behavior that corresponds to social norms is shown significantly more often. For the consolidation of a healthy lifestyle, it is therefore helpful to establish it as a norm in the immediate social environment of the target group.
Operational Readiness as a Military Norm
To achieve a sustainable increase in individual operational readiness, the principle of operational readiness should thus be embedded more firmly as a military norm within the Bundeswehr. In a corresponding incentive system, the incentive option (1) “social recognition” therefore has particular significance, as medals and career advantages can act as anchor points to consolidate the military norm “ operational readiness”. In addition to these incentives for soldiers, analogue incentives should be established at the (higher-)command level (e. g., department quality seals) to achieve sustainable changes at both personnel- and executive level.
Conclusion
In conclusion, incentive systems can also be used within the Bundeswehr to improve health behavior and individual operational capability. Prerequisites for an effective incentive concept are, however, (i) a target group-oriented design of incentive options, (ii) the parallel implementation of consolidation measures, and (iii) the involvement of personnel and executive levels (see Figure 2).
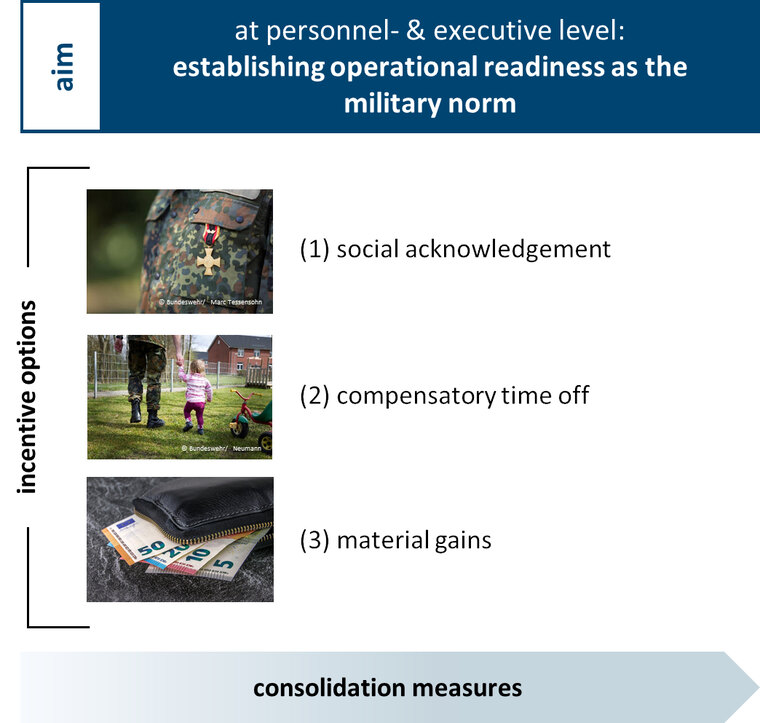
Fig. 2: Prerequisites for an effective incentive system to improve health behavior and individual operational readiness in the Bundeswehr are the target-group-oriented design of incentive options, the parallel implementation of consolidation measures and the involvement of personnel and executive levels.
References
- Bundesministerium der Verteidigung: A1-224/0-1: Sport und Körperliche Leistungsfähigkeit [Military regulation: Sport and physical performance].
- Bull FC, Armstrong TP, Dixon T et al.: Physical inactivity (Chapter 10). In: Ezzati M, Lopez AD, Rodgers A, Murray Christopher J. L. (eds.): Comparative quantification of heatlh risks. Global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization 2004; 729–881. mehr lesen
- Crespin DJ, Abraham JM, Rothman AJ: The effect of participation in an incentive-based wellness program on self-reported exercise. Prev Med 2016; 82: 92-98. mehr lesen
- Elbe M: Motivation und Karriereorientierung von Soldatinnen und Soldaten: Dienstgradgruppen im Vergleich: eine Analyse auf Grundlage der Personalbefragung 2016 (Forschungsbericht Nummer 121, Projektnummer 7130-01) [Motivation and career orientation of female and male soldiers: Rank groups in comparison: an analysis based on the 2016 personnel survey. Research Report, Project Number 7130-01]. Potsdam: Bundeswehr Centre for Military History and Social Sciences. mehr lesen
- Jacowitz KE, Kahneman D: Measures of anchoring in estimation tasks. Pers Soc Psychol Bull 1995; 21(11): 1161-1166. mehr lesen
- Jordan S, Lippe E von der: Prevention Programmes – Who takes part? GBE Kompakt 2012; 3(5): 1-9. mehr lesen
- Jordan S, Lippe E von der, Hagen C: Verhaltenspräventive Maßnahmen zur Ernährung, Bewegung und Entspannung. [Preventive behavioral interventions for nutrition, exercise and relaxation] In: Robert Koch Institut (ed.): Daten und Fakten: Ergebnisse der Studie »Gesundheit in Deutschland aktuell 2009. Gesundheitsberichterstattung des Bundes [Data and Facts: Results of the GEDA-study 2009. German federal health reporting] Berlin: Robert Koch Institut 2011; 23-34. mehr lesen
- Jordan S, Lippe E von der, Starker A, Hoebel J, Franke A: Factors Influencing Participation in Financial Incentive Programmes of Health Insurance Funds. Results of the Study “German Health Update“. Gesundheitswesen 2015; 77(11): 861-868. mehr lesen
- Kahneman D, Tversky A: Prospect theory: An analysis of decision under risk. Econometrica 1979; 47(2): 263. mehr lesen
- Lange C, Finger JD: Health-related behaviour in Europe – A comparison of selected indicators for Germany and the European Union. Journal of Health Monitoring 2017; 2 (2): 1-20 mehr lesen
- Leyk D: The problem of “individual operational readiness”: facts and options. WMM 2021; 65(3-4): 122-126. mehr lesen
- Leyk D, Rohde U, Hartmann ND et al.: Results of a workplace health campaign. What can be achieved? Dtsch Ärztebl Int 2014; 111 (18): 320-327. mehr lesen
- Leyk D, Rüther T, Witzki A et al.: Physical fitness, weight, smoking, and exercise patterns in young adults. Dtsch Ärztebl Int 2012; 109(44): 737-745. mehr lesen
- Mantzari E, Vogt F, Shemilt I et al.: Personal financial incentives for changing habitual health-related behaviors: A systematic review and meta-analysis. Prev Med 2015; 75: 75-85. mehr lesen
- Stock S, Schmidt H, Büscher G et al.: Financial incentives in the German Statutory Health Insurance: new findings, new questions. Health policy 2010; 96 1): 51-56. mehr lesen
- World Health Organization (ed.): Noncommunicable diseases country profiles 2018. Geneva: World Health Organization. mehr lesen
For the Authors
Dr. Kristina Küper
Bundeswehr Institute for Preventive Medicine
Section A1 – Applied Health Promotion
Andernacher Str. 100, D-56070 Koblenz
E-Mail: kristinakueper@bundeswehr.org